Adipose-derived stem cell exosomes act as delivery vehicles of microRNAs in a dog model of chronic hepatitis
Zanolla et al., 2024
Elita Summary
This study looked at using autologous exosomes taken from a dog’s own fat-derived stem cells to treat chronic hepatitis and other inflammatory liver diseases. Exosomes are tiny packets released by stem cells that carry signals which help reduce inflammation and support tissue repair. In 295 dogs, treatment led to clear improvement in clinical signs and normalisation of key liver markers over six months, suggesting a promising cell-free option for managing liver disease.
Study Design at a Glance
- Sample: 295 dogs of various breeds diagnosed with severe degenerative hepatopathy (excluding cancer or hepatic vein thrombosis).
- Cell Source: Autologous: cADSCs were isolated from the dogs' own fat tissue.
- Treatment: Exosomes (0.2 mg of protein/mL per kg) suspended in PBS were transfused through the peripheral vein. Dogs underwent two injections of autologous exosomes at 30 and 180 days.
- Outcomes: Follow-up was conducted for six months (180 days).
- Clinical Signs: Assessed before the first injection and 30 days after the second injection.
- Biochemical Markers: Serum levels of ALT, ALP, AST, GGT, TSBA, BUN, and Albumin were measured before and after 30 and 180 days.
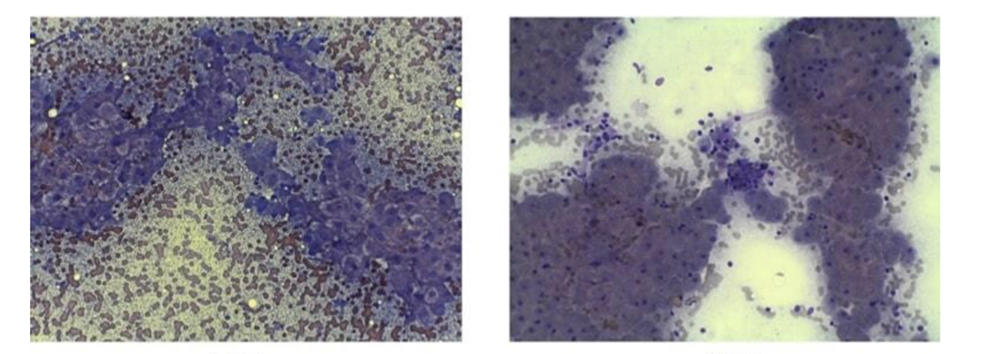
- Imaging/Histology: Hepatic cytology and sonoelastography were used to assess inflammation, fibrosis, and portal hypertension.
Key Clinical Outcomes
The treatment resulted in sustained improvement over the six-month period:
- Clinical Signs Recovery: Non-specific symptoms common in chronic hepatitis, such as decreased appetite (recovered in 96% of dogs) and lethargy/depression (recovered in 98% of dogs), showed a high rate of recovery 30 days after the second injection.
- Biochemical Marker Normalisation: All assessed biochemical markers associated with liver injury recovered by 180 days after exosome treatment.
- ALT and ALP (key liver enzymes) showed the greatest percentage change decrease after 180 days (ALT: 44% change; ALP: 42% change).
- Reduced Fibrosis and Inflammation: Cytological analysis showed that liver inflammation and fibrosis were strongly reduced after the second injection. Sonoelastography confirmed that fibrotic tissue was no longer visible, and portal vein blood flow was restored 180 days after the first injection.
- Safety: The treatment was deemed safe, complying with veterinary guidelines for autologous cell-based therapies.
Implications for Elita
This study represents a significant advancement by moving the treatment of chronic liver disease from live cell therapy to a cell-free exosome-based therapy.
- Validation of Autologous Exosomes: The success across a large cohort of 295 dogs demonstrates the clinical efficacy and safety of using autologous cADSC-exos to treat complex, long-term inflammatory hepatopathies.
- The "miRNA as Drug Delivery" Model: The work confirms that banked cells can be used to produce exosomes that act as delivery vehicles for specific, highly conserved miRNAs (like miR-199, let-7b, miR-21) responsible for therapeutic effects.
- Reinforcing the Need for Early Banking: The positive outcomes are predicated on using a patient’s own healthy cells for exosome production. This reinforces Elita’s core message: banking young, healthy cells is the proactive step that ensures access to the highest quality raw material for future personalised cell-free therapies.
