Effect of Adipose-Dervived Mesenchymal Stem and Regenerative Cells on Lameness in Dogs with Chronic Osteoarthritis of the Coxofemoral Joints: A Randomized, Double-Blinded, Multicenter Controlled Trial
Elita Summary
Stem Cells vs. Arthritis: What a Peer-Reviewed Study Tells Us (and What It Doesn’t)
At Elita, we closely monitor peer-reviewed studies in regenerative medicine to inform our approach and help shape future research directions here in Australia. As a stem cell bank, we’re particularly interested in trials that aim to assess real-world outcomes in companion animals, especially those that move beyond anecdote and into controlled study design.
One such study, published in Veterinary Therapeutics in 2007, represents an important early effort to evaluate the efficacy of autologous adipose-derived mesenchymal stem cell (AD-MSC) therapy in dogs with chronic osteoarthritis (OA) of the hip. While the dataset is limited, the design is robust, and the findings are worth revisiting as the field matures.
Study Design at a Glance
This was a randomised, double-blinded, placebo-controlled, multicentre trial involving 21 client-owned dogs with mild to moderate bilateral hip OA of at least six months' duration. Dogs were split into two groups: one received a single intra-articular (IA) injection of AD-MSCs into each hip joint; the other received a placebo (saline). All participants continued with stable NSAID therapy if already prescribed, but no other interventions were permitted during the study window.
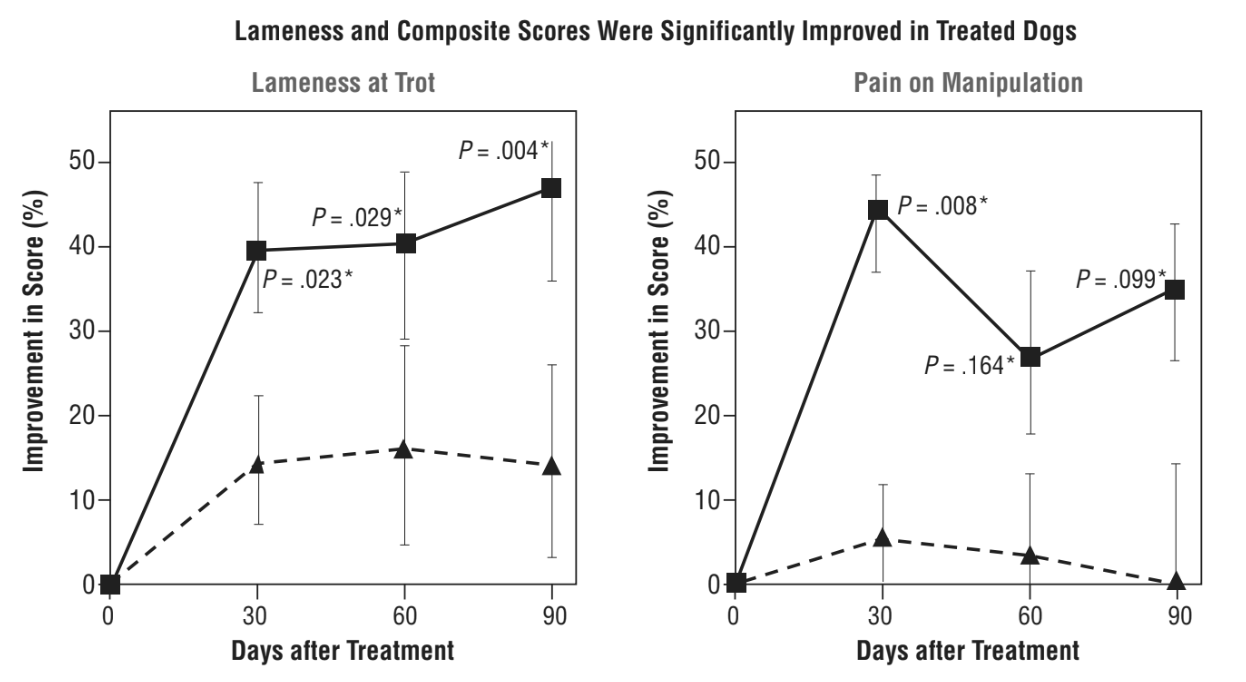
Veterinary assessments and owner surveys were conducted at baseline, and again at days 30, 60, and 90 post-injection. Clinical endpoints included lameness (walk and trot), pain on manipulation, range of motion, and a functional disability score.
What Did They Find?
Dogs treated with AD-MSCs showed statistically significant improvement across several clinician-assessed measures:
- Lameness (walk and trot)
- Pain on manipulation
- Range of motion
Notably, these improvements were observed from day 30 onwards and sustained through to day 90. The magnitude of improvement was sufficient in many cases to downgrade persistent lameness to intermittent, a clinically meaningful shift.
Functional disability scores also improved in treated dogs, but the high subjectivity of this measure and greater variance limited statistical confidence.
Owner surveys suggested perceived improvement in quality of life and mobility in the treatment group, although the sample was reduced due to protocol deviations and the results did not reach significance.
Importantly, no major adverse events were reported, and the treatment was well tolerated across the cohort.
Strengths of the Study
- Study design: Double-blinded and placebo-controlled trials are still rare in this space. The study's design lends real weight to its findings.
- Clear effect sizes: Several endpoints demonstrated strong clinical effect sizes, particularly for lameness at the trot, range of motion, and pain reduction.
- Safety profile: With no significant adverse reactions observed, the treatment appears well tolerated in a clinical setting.
-
Limitations (and Opportunities for Further Research)
- Small sample size: With only 18 dogs completing the study, the findings are not generalisable. Larger studies are needed to validate and standardise outcomes.
- Limited follow-up: A 90-day evaluation period captures only short-term outcomes. Long-term durability of treatment remains unassessed.
- Functional outcomes: While encouraging, improvements in functional disability were not statistically robust and could benefit from complementary objective measures such as force plate analysis.
- Owner data variability: Some owner-reported data were excluded due to protocol violations, reducing confidence in this aspect of the analysis.
- Further characterisation of the stromal vascular fraction: More research is needed on the particulars of the cell populations that accompany AD-MSCs.
Despite these limitations, the study remains significant as the first randomised, placebo-controlled clinical trial of stem cell therapy in dogs. It provides a foundational data point for the growing body of regenerative veterinary medicine.
Why It Matters to Us
While this is not definitive evidence of a "miracle cure," it does align with what many veterinarians have been reporting anecdotally: improvements in pain, mobility, and quality of life following autologous stem cell treatment.
At Elita, studies like this help shape our roadmap. They offer a glimpse of what’s possible, and underline the need for continued, larger-scale, ethically designed trials in the Australian context. As we build out our own veterinary partnerships, these are exactly the types of studies we aim to replicate and improve upon, with consistent data capture and long-term outcome tracking.
