Immunosuppression-enhancing effect of the administration of allogeneic canine adipose-derived mesenchymal stem cells (cA-MSCs) compared with autologous cA-MSCs in vitro
Elita Summary
As interest in allogeneic cell therapies grows, understanding how donor-derived stem cells compare to autologous options is critical, particularly in immunomodulatory contexts. This 2021 study by Wi et al. explored whether allogeneic canine adipose-derived MSCs (cA-MSCs) offer enhanced immunosuppressive effects compared to autologous MSCs in vitro. Their findings provide early, controlled evidence that could inform donor selection and therapeutic strategy in cases where immune modulation is central to the treatment goal.
Study Design at a Glance
- Objective:
- To compare the immunomodulatory effects of allogeneic versus autologous cA-MSCs on activated canine lymphocytes in vitro.
- Methods:
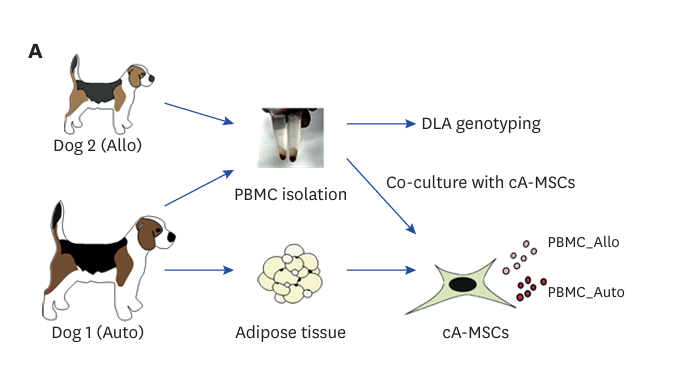
- MSCs were isolated from canine adipose tissue and either administered to the same donor (autologous) or to genetically unrelated dogs (allogeneic)
- Peripheral blood mononuclear cells (PBMCs) were isolated and stimulated with Concanavalin A to induce lymphocyte proliferation
- MSCs were co-cultured with stimulated PBMCs
- Lymphocyte proliferation, cytokine expression (IL-2, IL-4, IL-10, TGF-β, IFN-γ), and regulatory T cell (Treg) percentages were measured
Key Findings
- Lymphocyte suppression: Allogeneic cA-MSCs more significantly suppressed lymphocyte proliferation than autologous cA-MSCs.
- Treg induction: Allogeneic MSCs resulted in a greater increase in regulatory T cell (CD4⁺CD25⁺Foxp3⁺) populations.
- Cytokine profile:
- IL-10 and TGF-β levels were higher in the allogeneic group, supporting enhanced immunosuppression.
- Pro-inflammatory cytokines (IL-2, IFN-γ) were comparatively lower in the allogeneic co-cultures.
- Conclusion: Allogeneic cA-MSCs demonstrated stronger immunosuppressive effects in vitro, suggesting potential benefits for inflammatory or immune-mediated conditions.
Limitations
- In vitro only: Findings need validation in a clinical context. The in vivo behaviour of allogeneic cells may differ due to host immune responses, tissue homing, or rejection risks.
- Limited sample diversity: Donor and recipient dogs were not described in detail; factors like breed, age, and health status could influence immune interactions.
- No long-term functional outcomes: The study doesn’t assess the duration or durability of the immunosuppressive effects beyond the culture window.
Why It Matters to Us
This study adds to a growing body of in vitro evidence showing that autologous adipose-derived MSCs (AD-MSCs) may offer safer and more consistent immunomodulatory effects than allogeneic cells. While some immune-suppressive benefits were observed in the allogeneic group, the paper’s authors note the need for donor–recipient matching based on DLA type to ensure reliable outcomes, something not currently feasible in standard practice.
As the authors put it: “For safe, efficient, and consistent cA-MSC treatment in animal hospitals, it is necessary [to pursue] banking and database construction of cA-MSCs with variety of DLA types.”
At Elita, we believe autologous therapy remains the most practical and scalable approach for now, particularly in the absence of widespread donor matching infrastructure. This study supports our focus on building a bank of young, autologous stem cells where each pet is their own best match.
