Personalised-induced neural stem cell therapy: Generation, transplant, and safety in a large animal model
Elita Summary
This foundational study represents a significant advancement in personalised cell therapy for canines. For the first time, researchers successfully generated autologous induced neural stem cells (iNSCs) from the skin biopsies of healthy beagles. They then demonstrated that these cells could be safely implanted into the canine brain using two clinically relevant delivery methods: direct injection via a catheter and encapsulation in a biocompatible scaffold. This research not only confirmed the feasibility of manufacturing this personalised therapy at a large scale but also proved that the iNSCs could persist for several months without causing adverse side effects.
This study paves the way for future efficacy trials in canine patients with spontaneous brain tumors, bridging the critical gap between research in small animals and human clinical trials.
Study Design at a Glance
The study utilised four healthy, purpose-bred male beagles as a large animal model to test a new personalised stem cell therapy.
- Cell Source: Skin biopsies were collected from each dog. Fibroblasts from these biopsies were converted into tumour-seeking iNSCs and genetically engineered to carry therapeutic agents and a tracking agent (ferumoxytol).
- Delivery Methods: The canines were divided into two groups. Two dogs received iNSCs encapsulated in a biocompatible surgical matrix and implanted into a mock brain tumour resection cavity. The other two dogs received multiple doses of iNSCs delivered via a catheter into the brain's lateral ventricle.
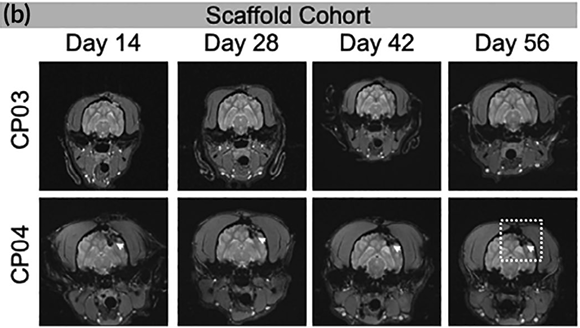
- Safety and Persistence Monitoring: The dogs were monitored for up to 84 days. Researchers assessed safety and toxicity using neurological exams, fluid analysis (blood, urine, cerebrospinal fluid), and histology. MRI was used to track the persistence and location of the implanted iNSCs.
Key Findings
This study provided compelling evidence for the safety and persistence of personalised iNSC therapy in a large animal model.
- Feasibility and Migration: The researchers successfully generated the first-ever canine iNSCs from skin fibroblasts. In laboratory tests, these cells were shown to efficiently migrate toward and kill tumour cells, mimicking the potent behaviour observed in human and mouse iNSCs.
- Safety and Toxicity: The iNSC therapy was generally well tolerated by all canines, with no abnormal tissue pathology attributed to the stem cells themselves. A major finding was that the observed adverse effects, including transient neutropenia and reproductive toxicity, were linked to the prodrug (valganciclovir, VGCV) used to activate one of the therapeutic agents, and not the iNSCs.
- Persistence: MRI confirmed the presence of the implanted iNSCs, showing that they persisted for at least 56 to 84 days post-implantation. The lack of a significant reduction in signal over this time suggests that the autologous nature of the cells allowed them to avoid a strong immune rejection.
- Clinically Relevant Delivery: Both the intracerebroventricular catheter and the scaffold delivery methods were found to be viable and safe for administering a large number of cells into the brain, a critical step toward clinical application.
Why This Matters Clinically
This study moves personalised neural stem cell therapy for dogs out of the theoretical and into the clinically achievable. For the first time, researchers have taken a dog’s own skin cells, converted them into tumour-targeting neural stem cells, and safely delivered them into the brain, without signs of rejection, and with cell persistence confirmed for over two months.
That’s not just a scientific milestone, it’s a clinical signal. It reinforces autologous cell banking as a foundational step for future neuro-oncology therapies and sets the stage for real treatment options in dogs with spontaneous gliomas.
With both scaffold and catheter delivery routes shown to be safe and clinically feasible, this research clears the path for therapeutic trials, not in rodents, but in real veterinary patients. For clinicians, it offers a glimpse of what’s coming: personalised, cell-based treatments for one of the most aggressive canine cancers.
Implications for Elita
At Elita, this study is a loud validation of everything we’re building:
- Bank once, treat many: A single skin sample can now be used to generate complex, tumour-targeting neural stem cells. It confirms the long-term value of autologous biobanking, especially for conditions that emerge years later.
- Beyond joints: While our early focus is on musculoskeletal and inflammatory conditions, this research expands what’s possible. It suggests that samples like the ones Elita banks today could one day support advanced neurological or oncology treatments.
- Clinical relevance, not theoretical hype: This study lays the essential groundwork, showing that autologous iNSCs can be manufactured, delivered safely, and persist in the brain. It moves the field one step closer to real therapeutic use. For us, it’s a reminder of why storing cells before illness matters, because when the science catches up, your pet already has what they need.
