The Use of Canine Mesenchymal Stem Cells for the Autologous Treatment of Osteoarthritis
Elita Summary
Unlocking a Dog's Own Healing Power: Adipose-Derived Stem Cells for Osteoarthritis
At Elita, we're committed to bringing the future of personalised medicine to pets across Australia. We keep a keen eye on global research to ensure our services are informed by the latest scientific advancements. We are particularly interested in studies that explore the therapeutic potential of a pet's own (autologous) mesenchymal stem cells (MSCs), especially for managing chronic conditions like osteoarthritis (OA) where traditional treatments can have limitations.
A compelling study published in Acta Veterinaria Hungarica in 2018 by Srzentić Dražilov and colleagues investigates the use of autologous, adipose-derived MSCs (AD-MSCs) for treating OA in dogs. This research highlights the significant clinical improvements observed after a single injection of these cells, underscoring their potential as a safe and effective therapy for this common degenerative joint disease.
Study Focus at a Glance
This study aimed to evaluate the effectiveness of using a dog’s own fat-derived stem cells to treat osteoarthritis. Key aspects include:
- Condition Treated: Osteoarthritis (OA) in canine patients.
- Source of Cells: Autologous (the dog's own) mesenchymal stem cells derived from adipose tissue (AD-MSCs).
- Treatment Protocol: A single injection of culture-expanded AD-MSCs directly into the symptomatic joint(s).
- Evaluation Periods:
- An initial evaluation at 30, 60, and 90 days post-treatment for all 10 dogs.
- An extended follow-up period of 1 to 4 years for 5 of these dogs.
- Outcome Measures: Clinical effects were assessed by a veterinarian for five key characteristics of OA: lameness at walk, lameness at trot, pain on manipulation, range of motion of the joint, and functional disability.
What Did They Find? The Therapeutic Promise of Autologous MSCs for OA
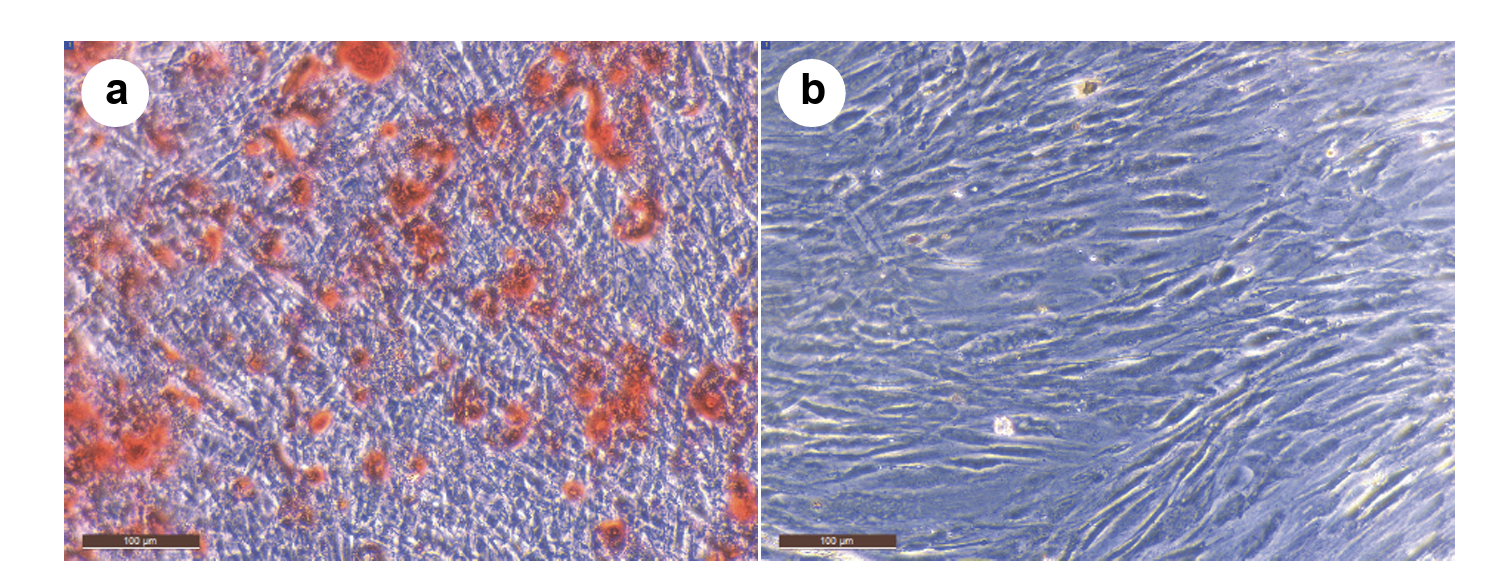
The study confirmed the "stemness" of the isolated cells, showing their ability to differentiate into bone and cartilage cell lineages, a crucial quality check for MSCs. The core findings on clinical efficacy were:
- Significant Short-Term Improvements (90 Days):
- All 10 dogs showed statistically significant improvement across all five assessed disabilities (lameness at walk, lameness at trot, pain on manipulation, range of motion, and functional disability) by day 90.
- The most substantial improvement was seen in "lameness at trot," with mean scores dropping dramatically.
- Encouraging Long-Lasting Effects (1-4 Years):
- In the 5 dogs available for extended follow-up, statistically significant improvement was maintained for "lameness at trot" and "range of motion of the joint" compared to their baseline scores before treatment.
- While not all measures retained statistical significance in this smaller group over the extended period, the mean scores for all characteristics still showed improvement compared to baseline, with "lameness at trot" again showing the largest positive change.
- Safety: Importantly, no adverse effects from the AD-MSC treatment were detected in any patient throughout the entire evaluation period.
The researchers concluded that using autologous AD-MSCs is a successful therapeutic approach for canine OA.
Strengths of the Study
- Long-Term Follow-Up: Provides valuable insights into the durability of the treatment effects, with the extended follow-up being one of the longest reported for MSCs in canine OA.
- Autologous Source: The use of a dog's own cells minimises risks of immune rejection and aligns with a personalised medicine approach.
- Comprehensive Clinical Assessment: Evaluation across multiple relevant clinical parameters provides a well-rounded view of treatment efficacy.
- Translational Relevance: The study highlights that dogs are an excellent model for human OA, meaning these findings may also inform human medical research.
Limitations (and Opportunities for Further Research)
The authors acknowledged several limitations common in such clinical research:
- Sample Size: The study involved a relatively small number of patients (10 dogs initially, 5 for long-term follow-up).
- Lack of a Control Group: The study did not include a blinded, placebo-controlled group, which can be challenging for logistical and ethical reasons in client-owned animal studies.
- Standardisation of Evaluation: The authors note the ongoing challenge in veterinary medicine regarding universally standardised functional evaluation scales, unlike in human medicine. Different methods for assessing parameters like range of motion exist across studies.
Why It Matters to Us
This research reinforces the core principles underpinning Elita: the remarkable, natural healing capabilities of a pet's own mesenchymal stem cells. The significant and lasting improvements seen in dogs with osteoarthritis, a chronic and often debilitating condition, highlight the value of MSC therapy.
For our veterinary partners and pet owners, this study provides further evidence supporting the consideration of autologous stem cell banking and therapy. Storing a pet's own AD-MSCs with Elita ensures that a safe, perfectly matched, and potent therapeutic option is readily available should conditions like osteoarthritis arise. This approach not only offers a promising avenue for enhancing a pet’s quality of life and mobility but also aligns with the best practice of personalised veterinary care, potentially reducing the reliance on long-term medications.
Studies like this one by Srzentić Dražilov et al. are crucial in demonstrating the tangible benefits of autologous AD-MSC therapy, paving the way for wider adoption of regenerative medicine in managing common orthopaedic conditions in our beloved companion animals. At Elita, we are proud to provide the means to access these innovative treatments, empowering veterinarians to offer cutting-edge care.
